Knee Pain Specialist in Nashik
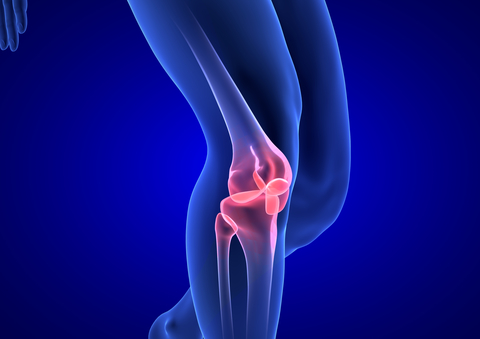
The knee is a joint that has three bones. The thigh bone (femur) meets the large shin bone (tibia) forming the main knee joint. The kneecap (patella) joins the femur to form the patellofemoral joint.
The knee joint is surrounded by a joint capsule with ligaments strapping the inner side and outer side of the joint, ‘medical & lateral collateral ligaments’. It also have ligaments crossing within the joint ‘cruciate ligaments’ which provide stability and strength to the knee joint.
The knee joint have a thickened cartilage pad between the femur and tibia,called as ‘meniscus’. It provides smooth surface for motion and absorbs the load of the body above the knee when standing.
The knee joint is surrounded by fluid-filled sacs called ‘bursae’, which reduces friction of the tendons on bones.
The knee joint is surrounded by a joint capsule with ligaments strapping the inner side and outer side of the joint, ‘medical & lateral collateral ligaments’. It also have ligaments crossing within the joint ‘cruciate ligaments’ which provide stability and strength to the knee joint.
The knee joint have a thickened cartilage pad between the femur and tibia,called as ‘meniscus’. It provides smooth surface for motion and absorbs the load of the body above the knee when standing.
The knee joint is surrounded by fluid-filled sacs called ‘bursae’, which reduces friction of the tendons on bones.
The large muscles of the thigh move the knee. In the front of the thigh, the quadriceps muscles extend the knee joint. In the back of the thigh, the hamstring muscles flex the knee. The knee also rotates slightly under guidance of specific muscles of the thigh.
Knee pain causes:
The most common reason for knee pain in 40 plus age is wear and tear in the knee joint, known
as Osteoarthritis. Osteoarthritis (OA) is degenerative joint disease in which the articular
cartilage and subchondral bone gets degenerated . When the cartilage thins, your bones rub
against each other and the lining of your joints, which is full of nerves and sensitive to pain.
steoarthritis develops earlier in former athletes who suffered knee injuries during their youth.
Its early symptoms are pain and stiffness in the morning or after strenuous activity. Morning stiffness usually resolves in less than an hour. Pain around the joint that increases with weight bearing and movement and improves with rest is the commonest presenting symptom.
Clinical signs are tenderness, crepitus, joint effusion, decreased range of movement, deformity of joint etc. X-ray shows decreased joint space, osteophytes(extra bone) formation and osteoporosis of subchondral bone.
Prevention & Care: In knee pain, one should avoid squatting, sitting on floor & climbing stairs. Do regular exercise.
Its early symptoms are pain and stiffness in the morning or after strenuous activity. Morning stiffness usually resolves in less than an hour. Pain around the joint that increases with weight bearing and movement and improves with rest is the commonest presenting symptom.
Clinical signs are tenderness, crepitus, joint effusion, decreased range of movement, deformity of joint etc. X-ray shows decreased joint space, osteophytes(extra bone) formation and osteoporosis of subchondral bone.
Prevention & Care: In knee pain, one should avoid squatting, sitting on floor & climbing stairs. Do regular exercise.
Treatments
I) Non-pharmacological therapy: Reduction of obesity, Quadriceps strengthening exercises, Deformity stabilization in which use of proper shoes transfers the load to the other
compartment and retards the disease process.
II) Pharmacological therapy: pain medications, agents which help in cartilage regeneration like chondroitin sulphate and gulcosamine sulphate.
III) Interventions/injections:
1. Injection of cortisone directly into the joint may temporarily help to relieve pain and swelling.
2. Viscosupplementation with artificial lubricant may increase the production of lubricant.
3. Pulsed radiofrequency stimulation and ablation of painful nerves may be helpful for some OA knees for longer term pain control. It uses electro-motive forces to encourage increased nutrient transport and recovery of the sensitized nerves. Once accurate placement of the RF needle on the nerve, it allows for obliteration of pain and surrounding supporting structures (muscles) to recover. Once the pain cycle is broken, the original painful joint is rehabilitated under active physiotherapy.
4. Prolotherapy and Prolozone Therapy. It is a helpful adjunct to therapy by strengthening ligaments/tendons and tightening the loosened or distorted joints. Injection of tissue proliferants (like ozone, phenol, glycerin, dextrose etc.) inside the joint and around the joint reduces pain and it strengthen ligaments. It is also supposed to promote cartilage growth.
5. PRP (Platelet Reach Plasma) or Stem cell therapy- Like its usefulness in other degenarative diseases, it is useful in osteoarthritis of knee also.
II) Pharmacological therapy: pain medications, agents which help in cartilage regeneration like chondroitin sulphate and gulcosamine sulphate.
III) Interventions/injections:
1. Injection of cortisone directly into the joint may temporarily help to relieve pain and swelling.
2. Viscosupplementation with artificial lubricant may increase the production of lubricant.
3. Pulsed radiofrequency stimulation and ablation of painful nerves may be helpful for some OA knees for longer term pain control. It uses electro-motive forces to encourage increased nutrient transport and recovery of the sensitized nerves. Once accurate placement of the RF needle on the nerve, it allows for obliteration of pain and surrounding supporting structures (muscles) to recover. Once the pain cycle is broken, the original painful joint is rehabilitated under active physiotherapy.
4. Prolotherapy and Prolozone Therapy. It is a helpful adjunct to therapy by strengthening ligaments/tendons and tightening the loosened or distorted joints. Injection of tissue proliferants (like ozone, phenol, glycerin, dextrose etc.) inside the joint and around the joint reduces pain and it strengthen ligaments. It is also supposed to promote cartilage growth.
5. PRP (Platelet Reach Plasma) or Stem cell therapy- Like its usefulness in other degenarative diseases, it is useful in osteoarthritis of knee also.


